Embolic Stroke: A Comprehensive Guide
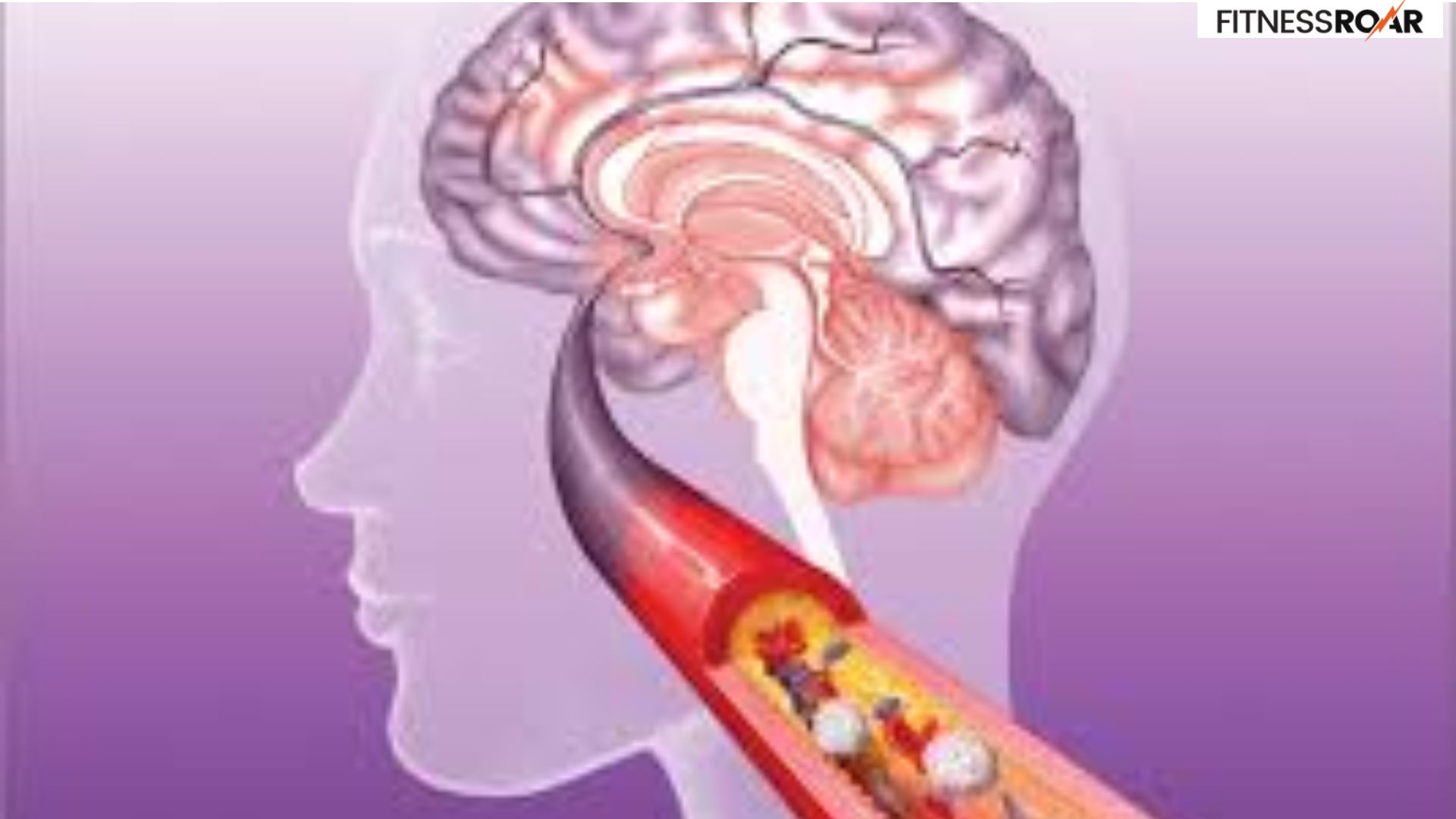
An embolic stroke is a type of stroke caused by a blockage in a blood vessel supplying the brain. This blockage occurs when a blood clot, formed elsewhere in the body, travels through the bloodstream and lodges in a narrower vessel within the brain. Deprived of oxygen and nutrients, brain cells in the affected area start to die, leading to stroke symptoms and potential long-term complications.
Understanding embolic strokes, including their symptoms, causes, diagnosis, and treatment options, is crucial for several reasons:
- Early Recognition: Recognizing the signs of an embolic stroke quickly allows for prompt medical attention. The sooner treatment is initiated, the better the chances of minimizing brain damage and improving recovery outcomes.
- Risk Factor Awareness: Knowing the causes of embolic strokes helps individuals identify and address their risk factors. This can significantly reduce the likelihood of experiencing a stroke in the first place.
- Effective Treatment: Accurate diagnosis allows healthcare professionals to determine the most appropriate treatment approach, potentially involving clot removal or medications to prevent further clotting.
- Improved Recovery: Understanding the rehabilitation process after an embolic stroke empowers individuals to actively participate in their recovery, potentially regaining lost function and improving their quality of life.
By shedding light on embolic strokes, we can empower ourselves and others to take preventive measures, recognize warning signs, and seek timely treatment, ultimately leading to better stroke outcomes.
Also Read: 5 Signs You’re Sleep Deprived
Symptoms of an Embolic Stroke

Embolic strokes are notorious for their sudden onset. One moment you might feel perfectly fine, and the next, you experience a cascade of neurological symptoms. Recognizing these symptoms quickly is vital for minimizing brain damage.
Sudden Onset – Acting FAST
The acronym FAST serves as a helpful memory tool to identify the telltale signs of a stroke, including embolic strokes:
F – Face Drooping: Does one side of the face appear numb or droop? Can the person smile evenly?
A – Arm Weakness: Can the person raise both arms equally? Is one arm noticeably weak or numb?
S – Speech Difficulty: Is the person’s speech slurred or difficult to understand? Can they form complete sentences?
T – Time to Call Emergency Services: If you observe any of these signs, call emergency services immediately. Time is brain tissue, and getting prompt medical attention is crucial.
While FAST provides a framework, other symptoms associated with embolic strokes include:
- Vision Problems: Sudden blurred vision, double vision, or complete loss of vision in one or both eyes.
- Balance and Coordination Issues: Difficulty walking, dizziness, or loss of coordination.
- Severe Headache: A sudden and severe headache, often described as the “worst headache of your life.”
- Confusion or Difficulty Understanding: The person may become confused, disoriented, or unable to follow instructions.
It’s important to remember that even if the symptoms appear mild or temporary, they could be a sign of an impending stroke. Don’t hesitate to call emergency services. Even if it turns out not to be a stroke, it’s always better to be safe than sorry. Early intervention can significantly improve the outcome.
Also Read: Why Vitamin D Levels Are Important
Causes of Embolic Strokes
An embolic stroke occurs when a blood clot, formed elsewhere in the body, travels through the bloodstream and gets lodged in a narrower artery within the brain. This clot, called an embolus, acts like a plug, cutting off blood flow and starving brain cells of oxygen and nutrients.
Several underlying conditions can contribute to the formation of emboli that lead to strokes:
- Atrial Fibrillation (AFib): This irregular heartbeat can cause blood to pool in the heart’s upper chambers, increasing the risk of clot formation. AFib is a major risk factor for embolic strokes.
- Heart Valve Disorders: Abnormal heart valves, whether narrowed or leaky, can create turbulent blood flow, promoting clot formation.
- Atherosclerosis: This condition involves the buildup of plaque (fatty deposits) within artery walls. Plaques can break off, forming emboli that travel to the brain.
Certain risk factors make individuals more susceptible to developing embolic strokes:
- High Blood Pressure: Uncontrolled hypertension damages blood vessel walls, making them more prone to plaque buildup and potential clot formation.
- High Cholesterol: Elevated cholesterol levels contribute to atherosclerosis, increasing the risk of emboli.
- Diabetes: Diabetes disrupts blood flow and can increase blood clotting tendencies.
- Smoking: Smoking damages blood vessels and promotes inflammation, both of which contribute to stroke risk.
- Obesity: Excess weight puts a strain on the cardiovascular system and increases the risk of developing conditions like diabetes and high blood pressure, which in turn elevate stroke risk.
- Previous Stroke or Transient Ischemic Attack (TIA): Having a prior stroke or TIA significantly increases the chances of experiencing another stroke, potentially embolic.
By understanding these underlying conditions and risk factors, individuals can work with their healthcare providers to implement preventive measures and potentially reduce their stroke risk.
Diagnosis of Embolic Strokes
A prompt and accurate diagnosis is crucial for maximizing recovery potential after an embolic stroke. Here’s a look at the diagnostic process:
Several medical procedures and tests can aid in diagnosing an embolic stroke:
- Neurological Examination: A doctor will assess your mental status, speech, vision, coordination, and muscle strength to identify any neurological deficits.
- Brain Imaging: Imaging tests like CT scans and MRIs create detailed pictures of the brain, helping to differentiate between an ischemic stroke (caused by a blockage) and a hemorrhagic stroke (caused by bleeding).
- Carotid Ultrasound: This non-invasive test uses sound waves to visualize the carotid arteries in the neck for signs of blockage or narrowing.
- Echocardiogram: This uses sound waves to examine the heart, looking for abnormalities like AFib or blood clots that could be a source of emboli.
- Angiography: In some cases, a cerebral angiogram, which involves injecting a contrast dye into the arteries, might be used to get a more detailed picture of the blood vessels in the brain and neck.
A timely diagnosis allows for the initiation of treatment as soon as possible. In certain cases, clot-removal procedures might be an option, but these are typically time-sensitive. The sooner the blockage is addressed, the better the chances of minimizing brain damage and improving long-term outcomes.
While embolic strokes share some symptoms with other stroke types, some key distinctions exist:
- Onset: Embolic strokes often have a sudden and dramatic onset, whereas other strokes might develop gradually.
- Imaging Findings: Brain imaging can reveal specific patterns of brain damage that might suggest an embolic stroke.
- Source Identification: Tests like echocardiograms can help identify the source of the embolus, which is a hallmark of embolic strokes.
An accurate diagnosis helps healthcare professionals tailor treatment strategies specific to the type of stroke, potentially improving the effectiveness of the intervention.
Also Read: Basic Tips for Winter Skin Care
In Crux
Knowledge is power, especially when it comes to stroke prevention.
By staying informed, taking preventive measures, and seeking help when needed, we can all play a role in reducing the burden of embolic strokes and their devastating consequences.
How much did you like Our detailed Embolic Strokes: Symptoms, Causes, Treatment? Please share your view in the comment box. Also, please share these Blogs with your friends on social media.
Recommended














