What is Fistulotomy? Understanding Procedure
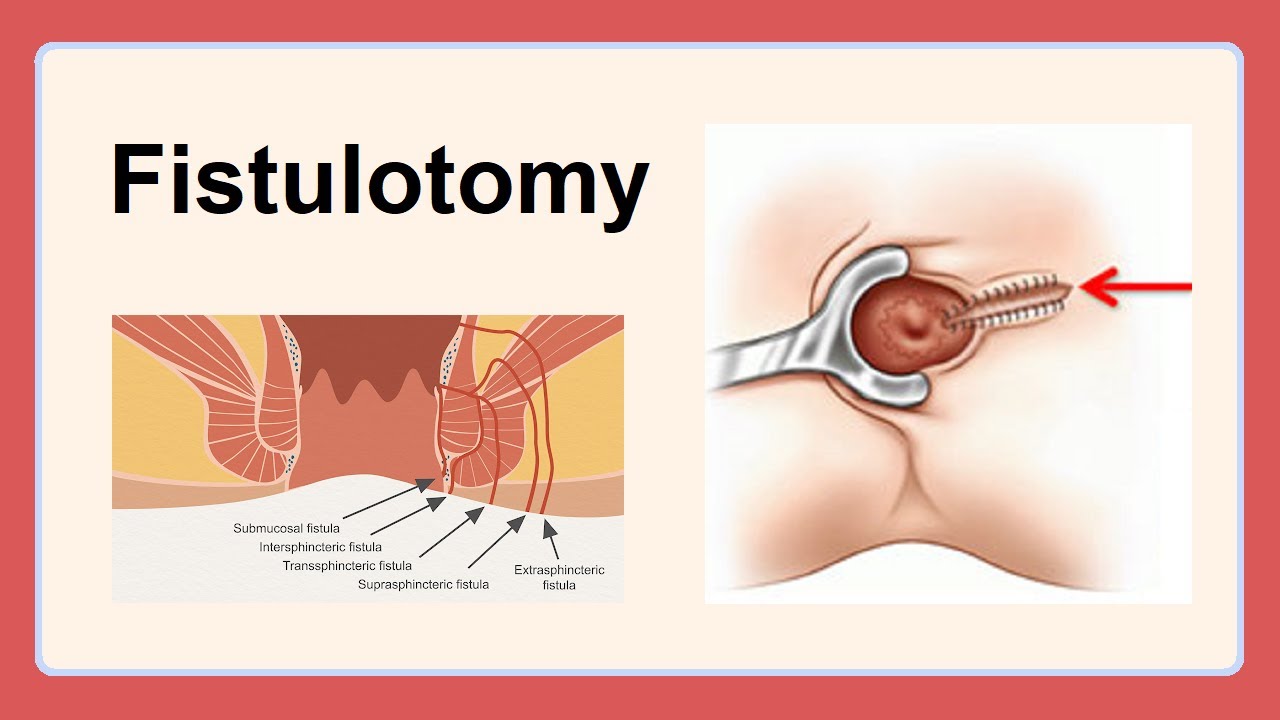
A fistulotomy is a surgical procedure used to treat an anal fistula. An anal fistula is an abnormal tunnel that connects the anal canal (the end of the large intestine) to the skin around the anus. This tunnel can cause pain, discomfort, and discharge.
A fistulotomy involves making an incision along the entire length of the fistula to open it up and allow it to heal from the inside out. This is typically an outpatient procedure, meaning you won’t need to stay overnight in the hospital.
Anal fistulas can be a persistent and uncomfortable condition. While fistulotomy is a common and effective treatment, it’s not always the right option for everyone. There are other surgical procedures available, and the best choice for you will depend on the specific characteristics of your fistula.
Understanding the different treatment options allows you to:
- Make informed decisions: By knowing the pros and cons of each procedure, you can discuss your options with your doctor and choose the treatment that best fits your needs and preferences.
- Prepare for the procedure: Once you know what type of surgery you’ll be having, you can ask questions about what to expect before, during, and after the procedure.
- Manage expectations: Different procedures have different success rates and recovery times. Understanding these factors can help you set realistic expectations for your treatment.
Also Read: Healthy Vegetable Juices for Summers
Fistulotomy Procedure
A fistulotomy is typically performed on an outpatient basis under either general anesthesia (you’ll be completely asleep) or spinal anesthesia (you’ll be awake but numb from the waist down). Here’s a general breakdown of the steps involved:
Preparation: You’ll be prepped for surgery with an intravenous (IV) line inserted into your arm for administering fluids and medications. The surgical area will be cleaned and sterilized.
Fistula identification: The surgeon will carefully examine the fistula to determine its location, depth, and course. This may involve using a special probe to trace the tunnel’s path.
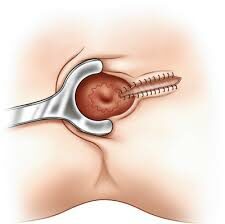
Incision: The surgeon will make an incision along the entire length of the fistula tract. The goal is to open the entire tunnel and allow complete drainage and healing.
Sphincter muscle preservation: Whenever possible, the surgeon will strive to preserve the anal sphincter muscles. These muscles control bowel movements, and damaging them can lead to incontinence.
Cleaning and packing: The opened fistula tract will be thoroughly cleaned to remove any debris or infection. In some cases, the surgeon may pack the wound with gauze to help it heal from the bottom up.
Closure (optional): Depending on the specific situation, the surgeon may leave the wound open to heal naturally or close it with stitches.
Anesthesia: The choice of anesthesia depends on several factors, including the complexity of the fistula, your overall health, and your doctor’s preference.
- General anesthesia: This is preferred for more complex fistulas or if you have anxiety about the procedure.
- Spinal anesthesia: This allows you to remain awake during the surgery but numbs the lower half of your body.
- Surgical techniques: There are slight variations in how the incision is made depending on the location and complexity of the fistula. Some common techniques include:
- Lay open technique: This involves making a single, straight incision that completely opens the fistula tract.
- Horseshoe technique: This creates a curved incision that follows the path of the fistula.
The best surgical technique for your specific case will be determined by your surgeon based on the details of your fistula.
Also Read: Surprising Benefits of Organic Milk
Recovery Process
Following a fistulotomy, recovery typically involves a combination of pain management, wound care, and lifestyle modifications to promote healing and prevent complications.
Immediate post-operative care
- Pain management: You’ll likely experience some pain and discomfort after surgery. Your doctor will prescribe pain medication to help manage this.
- Sitz baths: Taking warm sitz baths several times a day can help soothe pain and promote healing. A sitz bath involves sitting in a few inches of warm water (not hot) for 10-15 minutes.
- Wound care: You’ll receive specific instructions on caring for your wound, including cleaning and dressing changes. It’s crucial to follow these instructions carefully to prevent infection.
- Diet and hydration: Maintaining a high-fiber diet and adequate fluid intake will help keep your stools soft and easier to pass, reducing strain on the healing area.
- Activity restrictions: You may need to limit strenuous activity for a week or two to allow for proper healing. However, some gentle walking is encouraged to prevent blood clots.
Long-term recovery expectations
- Timeline: Most people can return to their normal routine within 1-2 weeks after surgery. However, complete healing of the fistula tract can take several weeks or even months.
- Follow-up appointments: You’ll likely have follow-up appointments with your doctor to monitor the healing process and address any concerns you may have.
- Success rates: Fistulotomy has a high success rate, with most people experiencing complete healing of the fistula. However, there’s a small chance of recurrence.
Tips for managing discomfort
- Pain medication: Take your pain medication as prescribed by your doctor.
- Sitz baths: Continue taking regular sitz baths as recommended by your doctor.
- Stool softeners: Consider using stool softeners to make bowel movements easier and less painful.
- Wear loose clothing: Wear loose-fitting clothing made from breathable fabrics to avoid irritation.
- Maintain good hygiene: Keep the anal area clean and dry to prevent infection.
- Avoid straining: Avoid straining during bowel movements, which can put pressure on the healing area.
- Rest: Get enough sleep and rest to allow your body to heal.
Additional tips
- Apply a cold compress to the area to reduce swelling and discomfort.
- Practice relaxation techniques like deep breathing or meditation to manage pain.
- Avoid lifting heavy objects until your doctor advises it’s safe.
- If you experience any signs of infection, such as increased pain, fever, or redness, contact your doctor immediately.
Following these tips and your doctor’s specific instructions will help you manage discomfort and promote optimal healing after a fistulotomy.
Risks and Complications
Fistulotomy is a generally safe procedure, but like any surgery, it carries some potential risks and complications.
Potential complications
- Infection: As with any surgery, there’s a risk of infection at the surgical site. This can be treated with antibiotics.
- Bleeding: Bleeding is a possibility, though usually minor.
- Incontinence: Incontinence of stool or gas is a potential complication, especially with complex fistulas that involve the sphincter muscles. The risk is relatively low with a skilled surgeon using sphincter-sparing techniques.
- Recurrence: There’s a small chance that the fistula may recur, especially with complex fistulas or those that were neglected for a long time.
- Narrowing of the anal canal (stricture): Scarring from the surgery can cause narrowing of the anal canal, making bowel movements difficult.
- Damage to nerves: In rare cases, nerves near the fistula tract can be damaged during surgery, leading to temporary or permanent numbness.
Ways to minimize risks
- Choosing an experienced surgeon: A board-certified colorectal surgeon with experience performing fistulotomies is crucial to minimize risks and optimize outcomes.
- Pre-operative discussion: Discussing your medical history and any concerns you have with your doctor beforehand allows them to take steps to minimize potential complications.
- Following post-operative instructions: Carefully following your doctor’s instructions regarding wound care, pain management, diet, and activity restrictions is essential to promote healing and prevent complications.
- Maintaining good hygiene: Proper hygiene practices after surgery help reduce the risk of infection.
By understanding the potential risks and taking steps to minimize them, you can feel more confident about undergoing a fistulotomy. If you experience any concerning symptoms after surgery, such as increased pain, fever, or difficulty controlling bowel movements, be sure to contact your doctor promptly.
Also Read: Best Teas for Effective Weight Loss
Success Rates
Fistulotomy boasts a high success rate, with most studies reporting closure rates between 80% and 98%. This means that a significant majority of people who undergo a fistulotomy experience complete healing of the fistula tract.
Several factors can influence the success rate of a fistulotomy:
- Type of fistula: Simple, low-transsphincteric fistulas generally have higher success rates compared to complex, high transsphincteric or horseshoe fistulas that involve the sphincter muscles].
- Surgical skill and experience: The expertise of the surgeon plays a significant role. A skilled surgeon experienced in performing fistulotomies can minimize the risk of complications and improve the chances of successful closure.
- Patient compliance: Following post-operative instructions regarding wound care, pain management, diet, and activity restrictions is crucial for optimal healing and reducing the risk of recurrence.
- Underlying medical conditions: Certain medical conditions, such as Crohn’s disease or compromised wound healing, can increase the risk of recurrence.
Recurrence rates: Even with a high success rate, there’s a small chance (around 5-15%) that the fistula may recur after a fistulotomy. This risk is higher for complex fistulas or those that were neglected for a long time.
If you’re considering a fistulotomy, discuss these factors with your doctor to understand your individual chances of success and potential risks. They can assess your specific situation and provide a more personalized outlook.
Candidacy for Fistulotomy
Fistulotomy is a good treatment option for many people with anal fistulas, but it’s not necessarily suitable for everyone. Here are some characteristics of ideal candidates for a fistulotomy:
- Simple fistula: The fistula is low-lying (not involving the sphincter muscles extensively) and has a straightforward tract that can be easily identified and opened.
- Good overall health: You are in good overall health and have no underlying medical conditions that could complicate healing.
- Realistic expectations: You understand the potential risks and limitations of the procedure and have realistic expectations for the recovery process.
- Ability to follow post-operative instructions: You are committed to following your doctor’s instructions regarding wound care, pain management, diet, and activity restrictions to promote healing and minimize complications.
Fistulotomy is often the preferred treatment for simple, low-transsphincteric fistulas because it’s a minimally invasive procedure with a high success rate and a lower risk of incontinence compared to other surgical options. However, other treatments may be considered in some cases:
Fistula seton placement: This is a minimally invasive procedure that involves placing a seton (a small piece of surgical thread) in the fistula tract to keep it open and drain infection. This may be used for complex fistulas or those involving the sphincter muscles to gradually reduce inflammation before definitive surgery like fistulotomy.
Fistulectomy: This is a more extensive surgery that involves removing the entire fistula tract, including the surrounding tissue. It may be necessary for complex, high transsphincteric fistulas or recurrent fistulas after fistulotomy.
Fibrin glue injection: This is a newer, minimally invasive technique that involves injecting a special glue into the fistula tract to close it. While promising, it’s still considered investigational and not widely available.
The best course of treatment for your anal fistula will depend on the specific characteristics of your condition, your overall health, and your doctor’s expertise. During a consultation, your doctor will discuss the various treatment options with you, considering the pros and cons of each approach in relation to your individual case.
In Crux
The information provided here offers a general overview of fistulotomy. If you suspect you have an anal fistula, it’s crucial to consult a healthcare professional for a proper diagnosis and personalized treatment plan.
By seeking professional medical advice, you can make informed decisions about your treatment and ensure the best possible outcome for your anal fistula.
How much did you like Our detailed What is Fistulotomy? Understanding Procedure? Please share your view in the comment box. Also, please share these Blogs with your friends on social media.
Recommended